Simulated RN™
Virtual Healthcare Agent

Understand the Problem: What do users need?
Understanding the users, their goals, and their challenges is key to designing a good system.
Users
Stakeholders
The stakeholders of the Simulated RN population consist of two groups: the hospital (e.g., executive groups, board of directors, passive leadership, managers, employees and healthcare providers) and the patients. All of the shareholders have a vested interest in a positive outcome related to the project. Members of the hospital group want their patients to enhance their understanding of treatment and healthcare options, because they want better outcomes and to increase patient satisfaction (Bickmore & Jack, 2010; Boudreaux, Ary, Mandry & McCabe, 2000). The patient group wants to be informed about their healthcare in a manner that supports their level of comprehension and learning style, so that they can be empowered to make informed decisions, which can lead to better health outcomes and satisfaction (U.S. Department of Health and Human Services, 2000; Clark, Drain, Gesell, Mylod, Kaldenberg & Hamilton, 2005).
Target Audience
In the exploratory study, the target audience will focus on shareholders specific to the maternity post-partum unit of the hospital, during the post-delivery or recovery phase of hospitalization. Primary Users: The primary user of the Simulated RN will be mothers of newborn infants and family members. Secondary Users: The secondary users of the system will be typical hospital staff members common to a typical post-partum unit. Users will consist of maternity experts: obstetricians, neonatologist, lactation consultants, certified nurse midwives, members of skilled nursing teams, and perhaps anesthesiologist.
The post-partum unit of the hospital was specifically targeted for this project for a key characteristic that may influence performance and design acceptance. It is anticipated that users from a technology driven generation will inevitably have more experience with virtual interactive interfaces, and therefore, will more likely accept such an interface as natural. As a result, women of childbearing ages provide a specific age range that increases the likelihood of previous contact with conventional technology.
Primary User Background Information
According to research by Livingston, Wang & Dockterman (2010), The New Demography of American Motherhood reported user related characteristics:
- Age: Mothers of newborns are older now than their counterparts were two decades ago. In 1990, teens had a higher share of all births (13%) than did women ages 35 and older (9%). In 2008, the reverse was true — 10% of births were to teens, compared with 14% to women ages 35 and older. Each race and ethnic group had a higher share of mothers of newborns in 2008 that are ages 35 and older, and a lower share that are teens, than in 1990.
- Marital Status: A record four-in-ten births (41%) were to unmarried women in 2008, including most births to women in their early 20s. In 1990, 28% of births were to unmarried women. The unmarried-mother share of births has increased most sharply for whites and Hispanics, although the highest share is for black women.
- Race and Ethnicity: White women made up 53% of mothers of newborns in 2008, down from 65% in 1990. The share of births to Hispanic women has grown dramatically, to one-in-four.
- Education: Most mothers of newborns (54%) had at least some college education in 2006, an increase from 41% in 1990. Among mothers of newborns who were ages 35 and older, 71% had at least some college education.
- Explaining the Trends: Trends cited above reflect a complex mix of demographic and behavioral factors that relate to various outcomes. For example, the higher share of college-educated mothers stems both from their rising birth rates and from women’s increasing educational attainment. The rise in births to unmarried women reflects both their rising birth rates and the shrinking share of adults who are married.
- Attitudes about Parenthood: When asked why they decided to have their first (or only) child, the overwhelming majority of parents (87%) answer, “The joy of having children.” But nearly half (47%) also say, “There wasn’t a reason; it just happened.” (Livingston, Wang & Dockterman, 2010, p.1).
Tasks
Generalized Hospital Procedures and Tasks
In a hospital, a discharge summary is a medical document used when a patient’s care transitions from one area of care to another, or to the home. The documentation of this process exists as part of the patient’s medical record. The purpose of this documentation is to provide communication between health care providers—generally, between physicians and nurses—related to a patient’s treatment and care.
The Joint Commission is an agency that provides evaluation, accreditation and certification for healthcare facilities in the United States. Joint Commission accreditation provides external validation of patient safety, clinical quality processes and standards for healthcare services. According to the standards set by the Joint Commission (Standard IM.6.10, EP 7), they mandate that six components must be present in all United States hospital discharge summaries. These components include (Joint Commission, 2012):
- Reason for hospitalization.
- Significant findings.
- Procedures and treatment provided.
- Patient’s discharge condition.
- Patient and family instructions (as appropriate).
- Attending physician’s signature.
The noteworthy component of the mandates associated with this initial prototype project relates to item five, the patient and family instructions. The patient and family instructions, often referred to as the discharge instructions, are a key component of the communication process between healthcare providers and patients. The distinction here is important to emphasize, because this communication is oriented with the patient and their ability to understand the instructions.
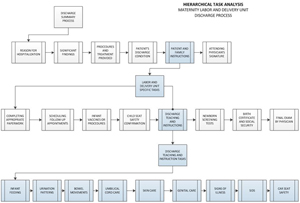
Post-Partum Unit Specific Tasks
The exploratory study will focus primarily on the post-partum unit of the hospital and mothers of healthy newborns. In a hospital, the physician will decide when it is safe for the mother and infant to be discharged from the hospital. Procedures and other tasks that need to be completed before they can be discharged include, discharge teaching and instructions, completing appropriate paperwork, scheduling of follow-up appointments, any vaccines or procedures for the infant (e.g., circumcision), child seat safety confirmation, newborn screening tests, birth certificate and Social Security registration, and the final physical exam by the physician.
Discharge Teaching and Instruction Procedural Topics
The framework for patient education content will be adopted utilizing recommendations provided by the American Academy of Family Physicians (AAFP), with specific attention given to the Discharge Procedures for Healthy Newborns (Langan, 2006). According to Robert Langan (2006), parents should receive training to give them the ability and confidence to care for their newborn in these key areas: properly feeding the infant, urination patterns, bowel movements, umbilical cord care, skin care, genital care, signs of illness, prevention of sudden infant death syndrome, car seat selection and proper use, and follow-up appointments made at discharge (p. 850).
User Tasks Summary
- Allow users to navigate the interface when they are prepared, or to locate desired information.
- Offer various instructional opportunities for the user to explore.
- Accommodate the users learning styles by providing them learning options.
Analysis
Communication and Comprehension Domain
Communication is essential for the effective delivery of healthcare (Paasche-Orlow, M. K., Parker, et al, 2005; Kripalani S, LeFevre F, Phillips, 2007; U.S. Department of Health and Human Services, 2000). Many medical studies demonstrated a correlation linking deficiencies related to communication and information transfer to implications related to patient safety and the continuity of care (Kripalani S, LeFevre F, Phillips, 2007). In fact, evidence shows patients often misinterpret or do not understand medical information given to them by clinicians (Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, 1999).
The data indicate that a large portion of the United States population lacks sufficient general literacy to effectively perform medical treatments (e.g., proper wound care, follow medication plan) it needs. According to the National Assessment of Adult Literacy, only 12 percent of adults have proficient health literacy to carryout proper self-care (Kirsch, Jungeblut & Jenkins 1993; U.S. Department of Health and Human Services, 2000). Studies have shown that 19 percent of discharged patients from hospitals have an incidence of an adverse event within 30 days following hospitalization and one third were preventable (Forster, Murff, Peterson, Gandhi & Bates, 2003). Many researchers have reported the most common factor influencing the frequency of adverse events relate to poor communication between hospital caregivers and the patient during the delivery of discharge instructions (Forster, Murff, Peterson, Gandhi & Bates, 2003). The economic consequences of inadequate health literacy are substantial, estimated to cost the United States $73 billion per year (U.S. Department of Health and Human Services, 2000). In 1994, adults with low health literacy averaged 6 percent more hospital visits, and stayed in the hospital almost 2 days longer than adults with higher health literacy skills (U.S. Department of Health and Human Services, 2000).
Patient Satisfaction Domain
In addition, research has demonstrated that the patient perception of discharge instructions are a powerful predictor of overall satisfaction (Boudreaux, Ary, Mandry & McCabe, 2000). Patients often find that the quality of discharge instructions do not match the quality of other services within the hospital (Clark, Drain, Gesell, Mylod, Kaldenberg & Hamilton, 2005).
Communication and Malpractice Lawsuits
Clinician-patient communication problems involved in malpractice lawsuits include explanation of diagnoses is inadequate, the explanation of treatment is inadequate, the patient feels ignored, clinician fails to understand perspective of patient or the relatives, clinician discounts or devalues views of patients or relatives, and the patient feels rushed (Weiss, 2003, p.24).
Summary of Breakdowns
A significant body of research literature substantiates that the most common breakdown that occurs in the discharge process relates to communication between the healthcare providers and the patient. Communication is a central element and the underlying factor related to other secondary breakdowns: patient comprehension and satisfaction. Therefore, it is predicted that improvement in the communication domain during the discharge instruction process will simultaneously improve patient comprehension and satisfaction. Therefore, the Simulated RN will strive to improve the discharge method by providing an interactive learning environment that enriches user tasks through enhanced communication.